Breast cancer is a significant global health issue affecting millions of women and men around the world. Breast Cancer Awareness, a movement that aims to educate, raise awareness, and promote early detection and treatment of this disease, has gained tremendous importance in recent years. It serves as a platform to inform individuals about the risk factors, symptoms, and available resources for prevention and support.
Breast Cancer Awareness campaigns strive to dispel myths and misconceptions surrounding the disease, empowering individuals to take charge of their health. By highlighting the importance of regular screenings, self-examinations, and understanding the signs and symptoms, these initiatives aim to catch breast cancer at its earliest stages when treatment options are most effective.
The impact of Breast Cancer Awareness extends beyond the individual level. It fosters a supportive community that encourages open dialogue, compassion, and solidarity among those affected by breast cancer and their loved ones. The movement unites healthcare professionals, researchers, survivors, and advocates, working collaboratively to improve outcomes, advance research, and provide a network of support for patients throughout their journey.
Breast Cancer Awareness is not limited to a single month or event; it is a year-round commitment to education, empowerment, and action. Various organizations, institutions, and communities across the globe organize awareness campaigns, fundraisers, and educational programs to reach diverse populations and emphasize the importance of early detection and timely treatment.
Through media campaigns, social media initiatives, educational materials, and community events, Breast Cancer Awareness endeavors to remove barriers to knowledge, encourage proactive healthcare behaviors, and provide support networks for those affected by breast cancer. It aims to ensure that every individual, regardless of their background or circumstances, has access to information, resources, and emotional support needed to navigate the challenges of breast cancer.
What Is Breast Cancer?
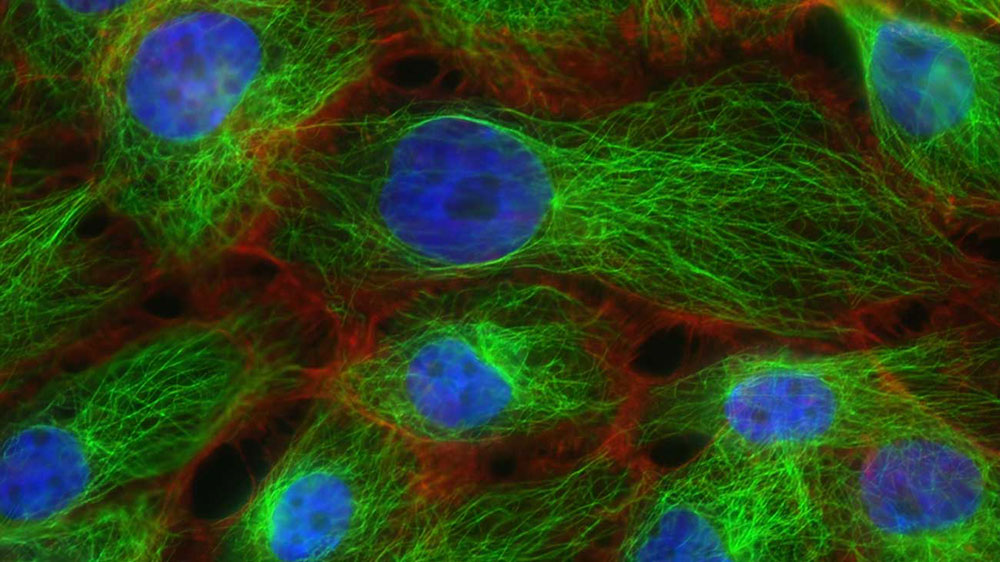
Breast cancer is a type of cancer that develops in the cells of the breast. It occurs when normal breast cells begin to grow uncontrollably, forming a malignant tumor. Over time, these cancerous cells can invade surrounding tissues and spread to other parts of the body.
Breast cancer can affect both women and men, although it is much more common in women. It is the most prevalent cancer among women worldwide. While the exact causes of breast cancer are not fully understood, several risk factors have been identified, including age, family history of the disease, certain genetic mutations (such as BRCA1 and BRCA2), hormonal factors, obesity, and exposure to certain chemicals or radiation.
Symptoms of breast cancer can vary, but some common signs include a lump or thickening in the breast or armpit, changes in breast size or shape, nipple discharge or inversion, skin dimpling or puckering, and redness or scaling of the breast skin. However, it’s important to note that not all breast lumps or changes indicate cancer, as many benign conditions can cause similar symptoms.
Early detection is crucial for the successful treatment of breast cancer. Regular screening methods, such as mammograms, clinical breast exams, and self-examinations, can help identify breast abnormalities at an early stage. If breast cancer is suspected, further diagnostic tests, such as a biopsy or imaging scans, may be performed to confirm the diagnosis.
Treatment for breast cancer depends on various factors, including the stage and type of cancer, as well as the individual’s overall health. Common treatment options include surgery (such as lumpectomy or mastectomy), radiation therapy, chemotherapy, hormone therapy, and targeted therapy. Treatment plans are often tailored to each patient’s specific situation and may involve a combination of these approaches.
Breast cancer research and advancements in treatment have significantly improved outcomes and survival rates. It is important for individuals to be aware of the risk factors, engage in regular screenings, and promptly seek medical attention if any concerning symptoms arise.
What Are the Types of Breast Cancer?
There are several types of breast cancer, which are classified based on where in the breast the cancer cells originate, the specific cells involved, and other characteristics of the tumor. The main types of breast cancer include:
- Ductal Carcinoma in Situ (DCIS): DCIS is a non-invasive breast cancer where abnormal cells are confined to the milk ducts and have not spread to surrounding breast tissue. It is considered an early-stage cancer and has a high cure rate.
- Invasive Ductal Carcinoma (IDC): IDC is the most common type of breast cancer, accounting for approximately 80% of cases. It begins in the milk ducts but invades the surrounding breast tissue. It can also spread to other parts of the body.
- Invasive Lobular Carcinoma (ILC): ILC starts in the milk-producing lobules of the breast and can spread to nearby tissues. It accounts for about 10-15% of invasive breast cancers.
- Inflammatory Breast Cancer (IBC): IBC is a rare and aggressive form of breast cancer. It typically does not present as a distinct lump but causes the breast to appear swollen, red, and inflamed. It progresses rapidly and requires immediate treatment.
- Triple-Negative Breast Cancer (TNBC): TNBC is characterized by the absence of estrogen receptor (ER), progesterone receptor (PR), and human epidermal growth factor receptor 2 (HER2). It tends to be more aggressive and is more challenging to treat compared to other types of breast cancer.
- Hormone Receptor-Positive (HR+) Breast Cancer: This type of breast cancer is characterized by the presence of hormone receptors, specifically estrogen receptors (ER) and/or progesterone receptors (PR), on the cancer cells. HR+ breast cancers may respond well to hormonal therapies.
- HER2-Positive Breast Cancer: HER2-positive breast cancer occurs when the cancer cells have an overexpression or amplification of the human epidermal growth factor receptor 2 (HER2) protein. It tends to be more aggressive, but targeted therapies that specifically block HER2 receptors have shown significant success in treatment.
These are the primary types of breast cancer, but there are also less common subtypes, such as mucinous carcinoma, tubular carcinoma, medullary carcinoma, and others. It’s important to note that the specific type and subtype of breast cancer are determined through diagnostic tests, such as biopsies and pathological analysis, which guide the treatment approach and prognosis for each individual.
What Are the Starting Signs and Symptoms of Breast Cancer?
Early-stage breast cancer may not cause noticeable symptoms in some cases. However, being aware of potential signs and symptoms can help individuals seek medical attention and undergo appropriate diagnostic tests. Here are some common starting signs and symptoms of breast cancer:
- Breast lump: The presence of a lump or thickening in the breast or armpit area is a common early sign of breast cancer. The lump may feel firm or have an irregular shape, but not all breast lumps are cancerous.
- Changes in breast size or shape: Unexplained changes in breast size, shape, or contour may indicate an underlying issue, including breast cancer. This can include swelling, asymmetry, or visible distortion.
- Nipple changes: Changes in the nipple can be a warning sign. These changes may include nipple inversion (when the nipple turns inward), flattening of the nipple, or a change in the direction of the nipple.
- Nipple discharge: Spontaneous nipple discharge, especially if it is bloody or occurs only in one breast, may indicate a problem. However, not all nipple discharge is cancerous, and some benign conditions can also cause it.
- Breast or nipple pain: While breast cancer is not typically associated with pain, some individuals may experience breast or nipple discomfort, tenderness, or localized pain. It’s important to note that most breast pain is unrelated to cancer.
- Changes in breast skin: Skin changes on the breast, such as redness, thickening, dimpling, or puckering (resembling an orange peel), can be an indication of breast cancer. Unusual warmth or a rash-like appearance on the breast should also be evaluated.
- Swollen lymph nodes: Swollen lymph nodes in the armpit or around the collarbone can be a sign that breast cancer has spread to the lymphatic system. However, swollen lymph nodes can also be caused by other conditions.
It’s important to keep in mind that these symptoms can be caused by various conditions, and experiencing them does not necessarily mean you have breast cancer. Many breast changes are benign, but it’s crucial to consult a healthcare professional if any concerning signs or symptoms persist or worsen.
Regular breast self-examinations, clinical breast exams by healthcare providers, and routine mammograms (as recommended based on age and risk factors) can help with early detection and prompt medical evaluation if any abnormalities are found.
What Are the Risk Factors of Breast Cancer?
There are several risk factors associated with the development of breast cancer. While having one or more of these risk factors does not guarantee the development of breast cancer, they can increase the likelihood. Here are some common risk factors:
- Gender: Being a woman is the most significant risk factor for breast cancer. Although men can also develop breast cancer, it is much more common in women.
- Age: The risk of breast cancer increases with age. Most breast cancers are diagnosed in women over the age of 50, with the majority occurring after menopause.
- Family history and genetics: Having a close relative (such as a mother, sister, or daughter) who has had breast cancer increases the risk. Certain inherited gene mutations, such as BRCA1 and BRCA2, significantly raise the risk of developing breast and ovarian cancer.
- Personal history of breast cancer: If an individual has previously had breast cancer in one breast, they have an increased risk of developing it in the other breast or having a recurrence.
- Dense breast tissue: Women with dense breast tissue (as seen on mammograms) have a higher risk of breast cancer. Dense breast tissue can also make it more challenging to detect small tumors on mammograms.
- Hormonal factors: Prolonged exposure to estrogen and progesterone can increase the risk of breast cancer. Factors that contribute to increased hormonal exposure include early onset of menstruation (before age 12), late menopause (after age 55), having the first child after the age of 30, never having been pregnant, and using hormone replacement therapy for an extended period.
- Lifestyle factors: Certain lifestyle choices and behaviors can impact breast cancer risk. These include excessive alcohol consumption, smoking, obesity or being overweight (especially after menopause), a sedentary lifestyle, and a diet high in saturated fats.
- Radiation exposure: Having undergone radiation therapy to the chest or breasts at a young age (such as for the treatment of Hodgkin’s lymphoma) increases the risk of developing breast cancer later in life.
- Hormonal contraceptives and hormone therapy: Some forms of hormonal contraceptives and long-term hormone replacement therapy (HRT) have been associated with a slightly increased risk of breast cancer. However, the overall risk is generally small and varies depending on the type and duration of use.
It’s important to note that having one or more risk factors does not mean an individual will develop breast cancer, and many people with breast cancer have no identifiable risk factors. Regular breast self-exams, clinical breast exams, and mammograms can aid in early detection, regardless of individual risk factors. It’s also crucial to discuss personal risk factors with a healthcare provider, who can provide personalized guidance and recommend appropriate screening and preventive measures.
What Are the Various Stages of Breast Cancer?
Breast cancer staging refers to the process of determining the extent and spread of the cancer within the breast and to nearby lymph nodes or other parts of the body. Staging helps healthcare professionals determine the appropriate treatment plan and assess the prognosis for an individual. The most commonly used breast cancer staging system is the TNM system, which stands for Tumor, Node, and Metastasis. Here are the stages of breast cancer:
Stage 0: This stage is known as carcinoma in situ, where abnormal cells are found only in the lining of the breast ducts (ductal carcinoma in situ or DCIS) or lobules (lobular carcinoma in situ or LCIS). At this stage, the cancer has not spread beyond its original location.
Stage I: At this stage, the cancer is invasive but is still relatively small and contained within the breast. It is divided into two subcategories:
- Stage IA: The tumor is 2 centimeters or smaller and has not spread to the lymph nodes.
- Stage IB: No tumor is found in the breast, but small groups of cancer cells are present in the lymph nodes, or the tumor is larger than 2 centimeters but has not spread to the lymph nodes.
Stage II: This stage is also divided into two subcategories:
- Stage IIA: There is no tumor in the breast, but cancer cells are found in 1-3 axillary lymph nodes, or the tumor is 2 centimeters or smaller and has spread to 1-3 axillary lymph nodes, or the tumor is larger than 2 centimeters but smaller than 5 centimeters and has not spread to the lymph nodes.
- Stage IIB: The tumor is larger than 2 centimeters but smaller than 5 centimeters and has spread to 1-3 axillary lymph nodes, or the tumor is larger than 5 centimeters but has not spread to the lymph nodes.
Stage III: Stage III breast cancer is considered locally advanced cancer. It is divided into three subcategories:
- Stage IIIA: The tumor may be any size and has spread to 4-9 axillary lymph nodes, or the tumor is larger than 5 centimeters and has spread to 1-3 axillary lymph nodes.
- Stage IIIB: The cancer may have spread to the chest wall or skin of the breast and may involve up to 9 axillary lymph nodes.
- Stage IIIC: The cancer has spread to 10 or more axillary lymph nodes, or has spread to lymph nodes above or below the collarbone, or has spread to lymph nodes in the axillary region or near the breastbone.
Stage IV: Stage IV breast cancer, also known as metastatic breast cancer, indicates that the cancer has spread to distant organs or distant lymph nodes. It may affect the bones, liver, lungs, brain, or other organs outside the breast.
In addition to the TNM system, other factors such as the tumor grade, hormone receptor status, and HER2 status are considered in determining the prognosis and treatment options for breast cancer.
It’s important to note that each individual’s case is unique, and staging may vary depending on various factors. Healthcare professionals use a combination of diagnostic tests, imaging scans, and pathological assessments to determine the stage of breast cancer accurately.
Can Men Get Breast Cancer?
Yes, men can get breast cancer, although it is much less common than in women. While breast cancer is predominantly diagnosed in women, men account for about 1% of all breast cancer cases. The anatomy of male breast tissue is different from female breast tissue, but men do have a small amount of breast tissue, which means they can develop breast cancer.
Risk factors for breast cancer in men include older age, family history of breast cancer, genetic mutations (such as BRCA2), radiation exposure, certain conditions that affect hormone levels (such as Klinefelter syndrome), liver disease, and obesity. Men with a family history of breast cancer or genetic mutations associated with the disease may have a higher risk.
The signs and symptoms of breast cancer in men are similar to those in women and can include a lump or thickening in the breast or armpit, changes in the nipple or breast skin, nipple discharge, and breast or nipple pain.
Because breast cancer in men is rare and often diagnosed at a later stage than in women, awareness and early detection are crucial. Men should be aware of any changes in their breast tissue and seek medical attention if they notice any abnormalities. Diagnostic tests such as mammograms, ultrasounds, and biopsies can help diagnose breast cancer in men.
Treatment for male breast cancer typically involves surgery, such as mastectomy (removal of the breast tissue) and lymph node dissection, along with radiation therapy, chemotherapy, hormone therapy, or targeted therapy, depending on the specific characteristics of the cancer.
It’s important for both men and women to be aware that breast cancer can affect anyone, and early detection and prompt medical care are essential for the best possible outcomes.
How Can I Minimize My Risks of Developing Breast Cancer?
While it’s not possible to completely eliminate the risk of developing breast cancer, there are several steps you can take to minimize your risk. Here are some strategies for reducing the risk of breast cancer:
- Maintain a healthy lifestyle: Adopting a healthy lifestyle can help reduce the risk of many diseases, including breast cancer. Focus on:
- Regular exercise: Engage in moderate to vigorous physical activity for at least 150 minutes per week. Exercise can help regulate hormone levels and maintain a healthy weight.
- Balanced diet: Consume a nutritious diet that includes a variety of fruits, vegetables, whole grains, lean proteins, and healthy fats. Limit the intake of processed foods, sugary drinks, and red meats.
- Maintain a healthy weight: Aim to achieve and maintain a healthy weight through a combination of a balanced diet and regular physical activity. Obesity is associated with an increased risk of breast cancer, especially in postmenopausal women.
- Limit alcohol consumption: Limit your alcohol intake or avoid it altogether. Excessive alcohol consumption is linked to an increased risk of breast cancer. If you drink, limit it to no more than one drink per day.
- Breastfeeding: If you have the opportunity and choose to do so, breastfeeding can provide benefits for both the mother and the baby. It has been shown to reduce the risk of breast cancer, particularly when done for a longer duration.
- Hormone therapy: If you are considering or currently using hormone replacement therapy (HRT) for menopausal symptoms, discuss the potential risks and benefits with your healthcare provider. Long-term use of combined estrogen and progestin hormone therapy may slightly increase the risk of breast cancer. However, the risk varies depending on factors such as the duration of use and individual characteristics.
- Know your family history: Be aware of your family history of breast cancer and other cancers. If you have a strong family history or certain genetic mutations, consider discussing this with a healthcare professional who can assess your risk and recommend appropriate screening or preventive measures.
- Regular screenings and self-exams: Follow recommended guidelines for breast cancer screenings. Mammograms, clinical breast exams, and breast self-exams can aid in early detection. Talk to your doctor about the appropriate screening schedule based on your age, risk factors, and individual circumstances.
- Stay informed and aware: Educate yourself about breast cancer, its signs and symptoms, and the latest guidelines for prevention and early detection. Stay up to date with advancements in breast cancer research and screening technologies.
It’s important to note that while these strategies can help reduce the risk of breast cancer, they do not guarantee prevention. Regular screenings and awareness remain crucial, as early detection provides the best chances of successful treatment. Consult with your healthcare provider for personalized guidance based on your individual risk factors and medical history.
Sources: www.cancer.org, www.breastcancer.org, www.mayoclinic.org, www.nationalbreastcancer.org. www.cdc.gov
Brought to you by Fomat Medical

